Enabling data exchange within and across health care organizations will require a paradigm shift towards the establishment within the environment of the health care provider, of a vendor neutral interoperability architecture that is modular, scalable, services based, and secure. This in turn requires a reframing of purchasers, vendors relationships, promoting a culture of partnership with the vendors and supported appropriately by health policy.
It is important for health systems to work collaboratively in order to develop shared technical requirements for procuring industry solutions, as well as in moving toward an agreed-upon open architecture layer for seamless end-to-end interoperability and data exchange in the long run.
The Interoperability Guide is intended to support healthcare providers in planning and procuring standards-based interoperable solutions. Such decisions are typically shared within the higher management executive level in the healthcare organisations responsible for procurement of equipment, ICT systems and related services. Thus, the Guide addresses Chief Executive and Information Officers. However, more management functions may be relevant in European hospitals and as such may be addressed by this Guide.
Several actors must be engaged and align efforts under national eHealth interoperability frameworks, in order to achieve meaningful sharing of health data across borders. The Guide assumes that such national frameworks exist and provide the necessary direction in terms of common standards to be deployed in the healthcare providers’ projects. However, even where such clear national guidance does not exist, there is still large potential for leveraging on international standards and interoperability specifications and European legal enablers for interoperability.
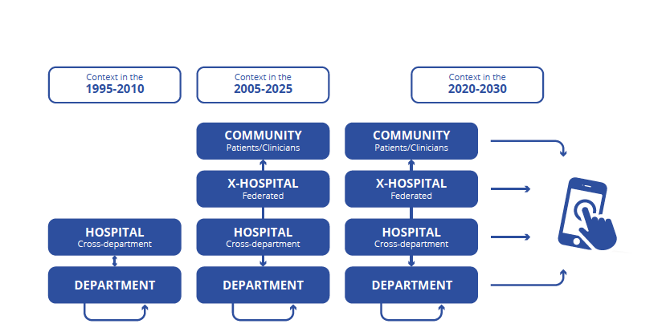
The focus of interoperability within hospitals has evolved over the past 30 years. Starting from the research type projects in the early 1990s until recently, where – depending on the hospital IT maturity and budget – the focus was mainly on digitising the key departments (laboratory, Radiology, Pharmacy, etc.) both internally and connecting them with the Hospital-wide information system (HIS). It has then slowly shifted to the integration of different hospitals within a geographical area or an organizational structure (e.g. hospital chains), while a first generation of regional/ national information exchange communities where established with hospitals broadly connected to their referral base of primary care providers and other specialized hospitals, in the current period that we can approximatively position around 2005-2025. Some early deployment across borders has also been successfully materialized, such as the European eHealth Digital Services Infrastructure (eHDSI). Most recently, a new wave where the role of mobile phone and personal health devices is emerging and likely to grow over the next 10 years. However, the hospital is increasingly faced with interoperability challenges that come from the external environment.
The challenges of interoperability for health care providers may be also differentiated by means of the level of information exchange involved:
It is time to inject some positivity back into interoperability. Often, it has been perceived as complex, messy and a source of frustration for CEOs and CIOs, but the smooth exchange of health information is a must and a critical business priority for healthcare organisations. Now is the moment to seize a fresh and strategic rethink and work towards change.
Health care providers can leverage EU standardization to meet their local needs in a global environment and use their buying power to stimulate competition within their local health ICT markets based on interoperability requirements. They should, furthermore, take legal advice to ensure that they are complying with the right legal basis, and ICT security advice on how to safeguard the data being used for care purposes and for research.
Health care providers can leverage on EU standardization to meet their local needs in a global environment and use their buying power to stimulate competition within their local health ICT markets based on interoperability requirements. They should, furthermore, take legal advice to ensure that they are complying with the right legal basis, and ICT security advice on how to safeguard the data being used for care purposes and for research. Read More
Learning Health Systems are systems where science, ICT, incentives, and culture are aligned for continuous improvement and innovation. High-quality EHR data is vital to the delivery of safe and effective patient care, enables the reuse of your data across your Learning Health System, strengthens your strategic and medical decision-making insights and improves your opportunities to scale up your participation in clinical research. You can stimulate and promote an interoperability culture amongst clinicians and other hospital staff engaged in data capture; develop competences for assessing data quality and maximising its reusability for other purposes such as reporting, learning and improving own practices and exchanging data with other organisations for care purposes or for clinical and public health research. Read more
Setting up and running internal systems, capable of capturing and securely exchanging health data within the hospital and with other organisations do not need to start from scratch. There are available assets in the form of common technical and semantic interoperability specifications, interoperability testing tools and platforms, guidelines, integrated frameworks, and semantic resources that can be exploited. The Guide provides a compass to finding relevant information. Read more
The eHealth Network has adopted Guidelines on “an interoperable eco-system for digital health and investment programmes for a new/updated generation of digital infrastructure in Europe”.
On their journey to interoperability, healthcare organisations should consider ICT procurement strategies and models that cater to interoperability and create an organisation-wide capacity. Read more
Communities of Practice (CoP) are primarily formed by people who engage in a process of collective learning in a domain of common interest where complementarity of skills, knowledge, perspectives and insights make for a sum that exceeds the result of their addition. To learn more and engage more closely with further developments, interested parties can join one of the committees of the participating organizations. Read more
Next chapter: